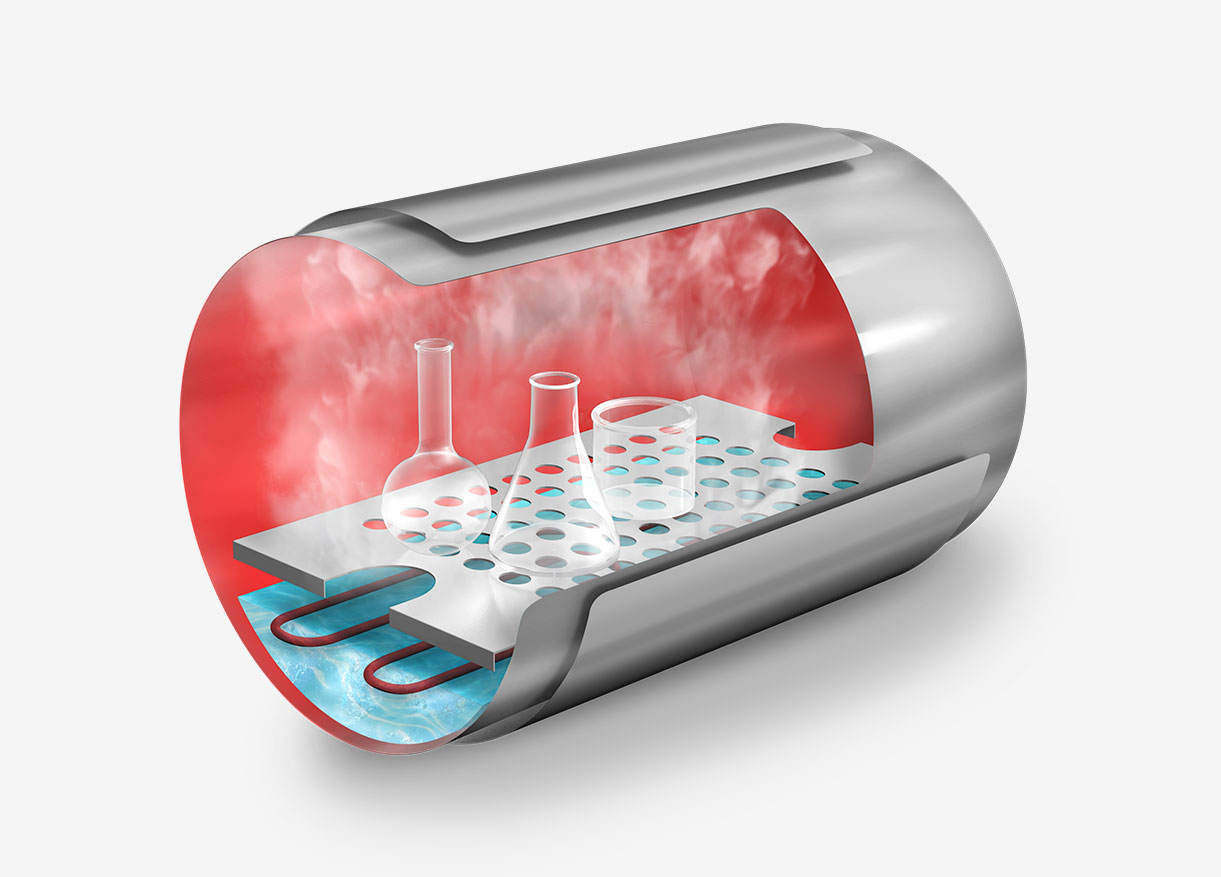
In sterilization processes, simply reaching the correct temperature inside the autoclave chamber is not enough. What truly matters is whether that temperature is also achieved within the load itself – especially when sterilizing liquids.
Direct monitoring inside the product ensures that all material has been properly sterilized, minimizing microbiological risks. Additionally, this measurement is key to calculating the F₀ value and optimizing cycles by reducing time without compromising the effectiveness of the process.
For this reason, PT-100 flexible probes have become an essential accessory in laboratories and facilities that demand precision, traceability, and validation in their sterilization processes.
What Are PT-100 Probes and How Do They Work?
PT-100 probes are temperature sensors based on the electrical resistance of platinum. The name indicates a resistance of 100 ohms at 0 °C. As the temperature changes, so does the resistance, enabling accurate readings even in demanding environments.
These probes are inserted directly into the load – for example, into a flask containing culture media – so they provide the actual temperature of the product, not just the surrounding environment. This distinction is particularly relevant in liquid loads, where heat penetrates more slowly.

Additionally, the use of PT-100 probes allows cycle control through the F₀ parameter (in compatible models), which represents the accumulated lethality of the process based on the time the sample remains at a specific temperature, using 121.1 °C as a reference.
Why Is It Crucial to Measure Inside the Product?
The temperature inside the sterilization chamber does not guarantee that the core of the sample has reached sterilization temperature. In liquids, there can be a significant thermal delay: steam may reach 121 °C while the liquid is still below 100 °C.
This lag can lead to false positives if the sterilization time is counted too early.
Measuring directly inside the product allows you to:
✅ Ensure the entire sample has been properly treated.
✅ Avoid microbiological risks.
✅ Validate and optimize cycles using the F₀ value.
PT-100 Probe Models Available from RAYPA
The flexible PT-100 probes offered by RAYPA are designed to ensure precise control of the sterilization process, especially when monitoring liquid loads. For optimal functionality and proper integration with the autoclave control system, these probes must be installed at the factory.
Flexible Probe for Classic Line Autoclaves
References: PT-2, PT-2-B, PT-2-AH and PT-2-B-AH
These probes are specifically designed to monitor the sterilization of liquid loads in autoclaves from RAYPA’s Classic line.

They are available in several versions, compatible with the AES, AE-DRY, AE-B, AHS-N, AHS-DRY, and AHS-B series, with probe lengths varying according to the specific autoclave model (60 mm for benchtop models, 120 mm for vertical models).
Main Benefits:
- Effective sterilization of liquids: The probe accurately measures temperature at the center of the liquid sample, ensuring that the required temperature is reached within the load. This significantly improves the reliability of the sterilization process.
- Prevention of boilover effects: Continuous monitoring of liquid temperature minimizes the risk of overheating and spills when opening the autoclave. This protects both the operator and other contents of the autoclave chamber.
- Optimization of sterilization processes: By simultaneously controlling the temperature in the chamber and inside the liquid, it provides more precise tracking of the F₀ value and cycle lethality. This facilitates more efficient sterilization, ensuring consistent results, regardless of the number or size of the processed containers.
Flexible Probe for Top Line Autoclaves
Reference: PT-2-TLV
Specifically recommended for accurate monitoring of liquid sterilization processes in RAYPA’s Top line autoclaves.

Compatible with RAYPA’s TLV-DUAL, TLV-PD, TLV-FA, and TLV-S autoclave models, all intended for critical applications requiring rigorous control. These units allow installation of up to two probes, enhancing versatility for monitoring. Some series, such as TLV-DUAL and TLV-FA, include one flexible probe as standard equipment.
Unlike the Classic line probes, the probe length varies depending on autoclave capacity and the specific needs of each sterilization process. This provides greater versatility, facilitating placement in various types of containers or different positions within the chamber.
Modes of use:
- Single flexible probe: Allows direct monitoring of the internal temperature of the liquid sample, initiating the sterilization phase only once the desired temperature is reached. Additionally, installation of this probe enables programming cycles based on the F₀ value, optimizing lethality control and offering greater process flexibility.
- Two flexible probes: Ideal for comparing conditions between different samples, especially when containers of varying sizes or positions within the chamber are used (such as upper and lower levels). The sterilization cycle starts only when both probes detect the required temperature, ensuring uniform treatment throughout the entire load.
Practical Recommendations for End Users
Choosing the right accessory to monitor temperature in an autoclave depends on the autoclave model, type of load, regulatory requirements, and process objectives.
👉 For liquids and culture media, a flexible PT-100 probe is always recommended.
👉 For heterogeneous loads, using two probes (in Top line models) helps identify cold spots and validate process uniformity.
👉 In laboratories subject to regulations such as GMP, FDA, or ISO 13485, it is essential to work with systems that enable F₀-based control, traceability, and report generation.
Common Errors When Using Probes in Autoclaves
Even with the appropriate probes, improper use can compromise the effectiveness of the sterilization process. Avoid the following mistakes:
🚫 Placing the probe in contact with the container wall (this distorts the measurement).
🚫 Using probes with damaged or uncalibrated cables.
🚫 Starting the cycle without confirming correct placement inside the sample.
🚫 Failing to verify probe compatibility with the autoclave model.
Expert tip
Always consult with the manufacturer or RAYPA’s technical support team to ensure you select accessories that are compatible with your specific model and application needs.
Do you have questions about which probe is best suited to your application? Our team of professionals is available to guide you and help you achieve safe, validated, and efficient sterilization.